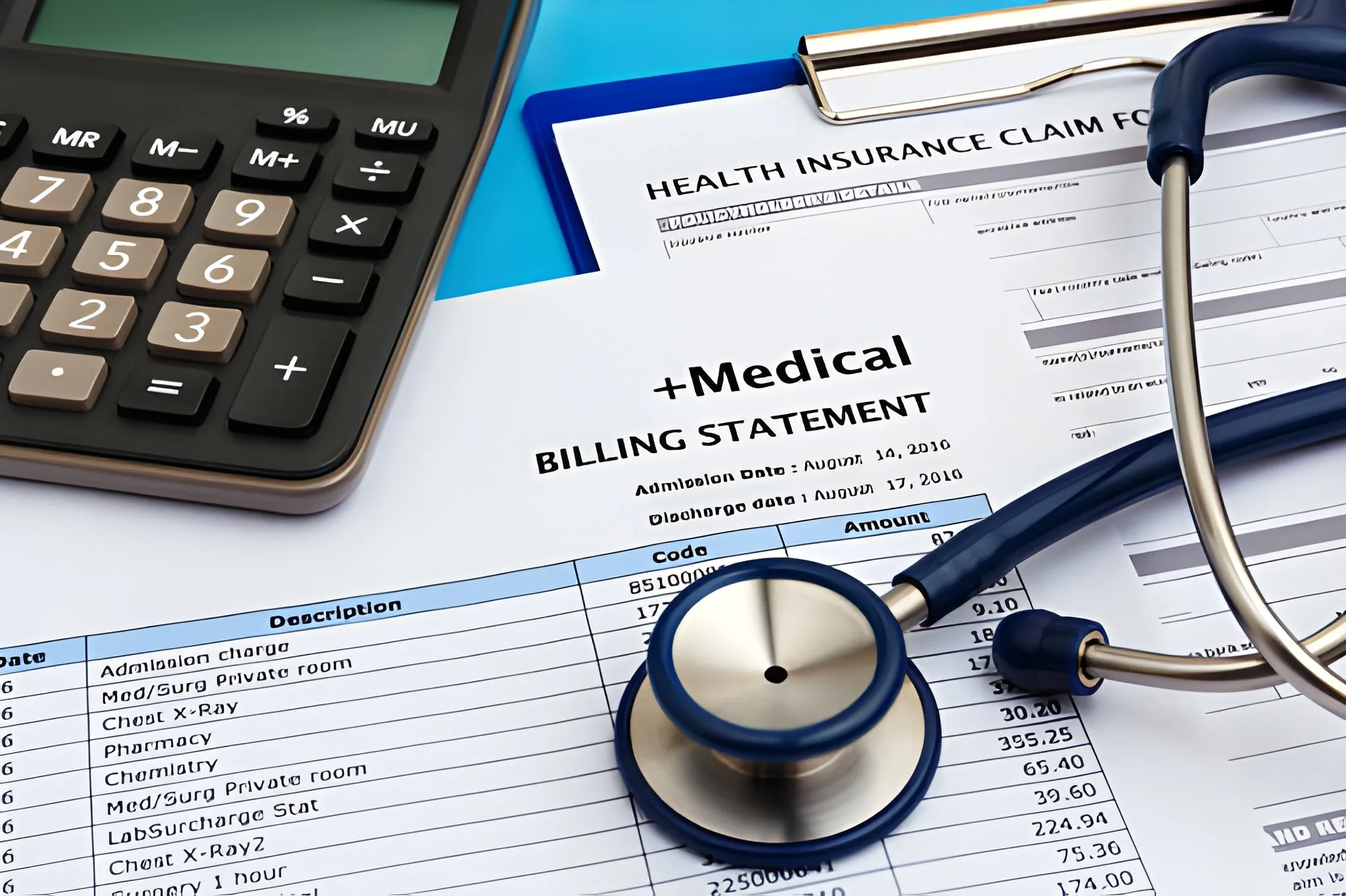
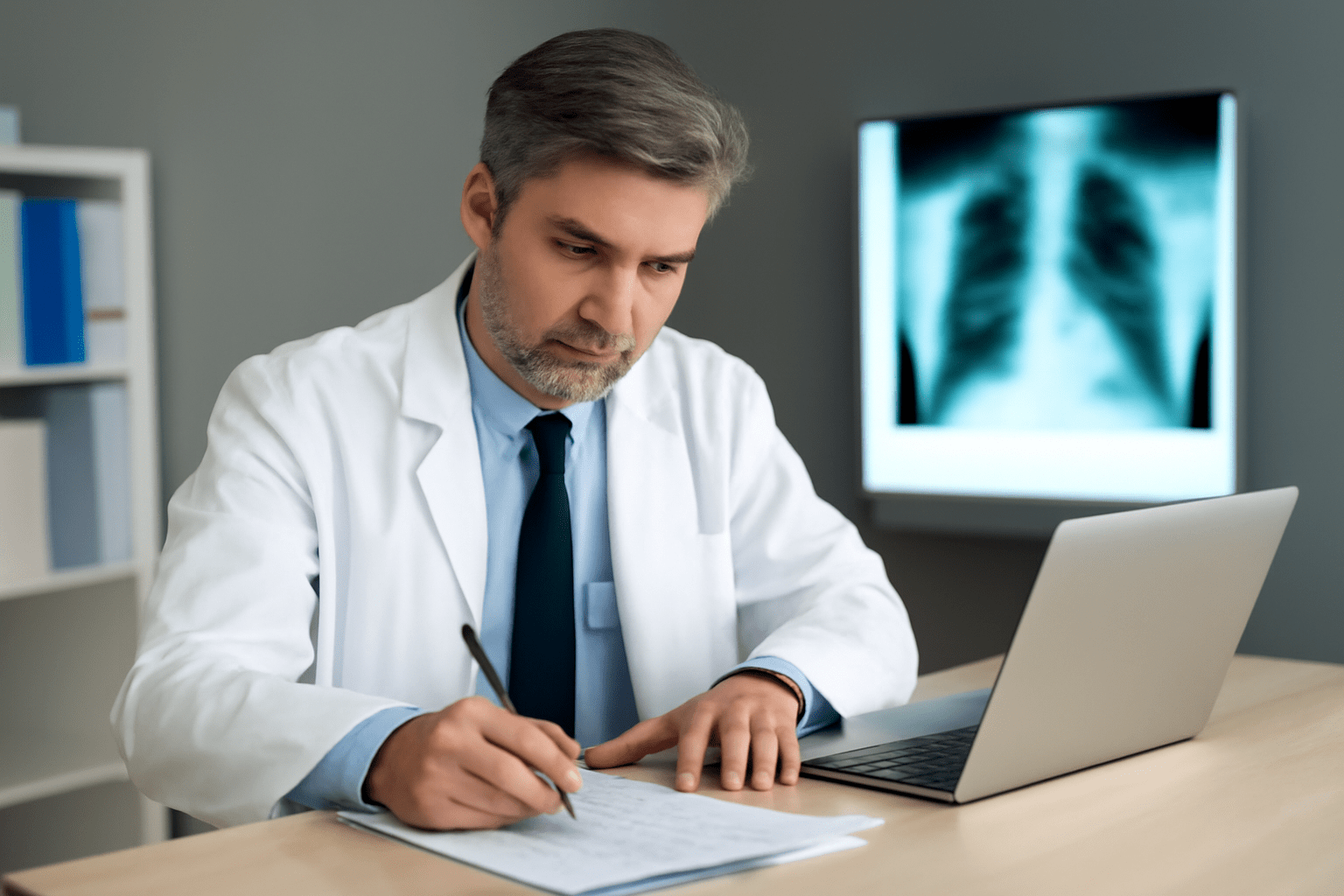
Pulmonology practices carry a denial rate sitting around 18%. That figure is nearly double the 5 to 10 percent baseline seen across most other specialties. The reason is not carelessness. Respiratory medicine involves procedures that overlap, codes that bundle incorrectly and diagnosis requirements that shift between payers constantly. A single...
Read More
Pulmonology Billing Codes: What Every Provider Must Know
Pulmonology practices carry a denial rate sitting around 18%. That figure is nearly double the 5 to 10 percent baseline seen across most other specialties. The reason is not carelessness.