Radiology billing can be one of the most complex aspects of medical practice management. With constantly evolving codes, intricate documentation requirements, and strict compliance standards, even experienced billing teams can fall into costly traps. These mistakes don’t just impact your bottom line but they can also lead to audit flags, claim denials, and delayed payments that disrupt your practice’s cash flow.
Understanding the most common radiology billing errors can help your practice avoid these pitfalls and maximize revenue. Let’s explore eight critical mistakes that could be costing your radiology practice thousands of dollars each month.
1. Incorrect Use of Modifier Codes
Modifier codes are essential in radiology medical billing, yet they’re frequently misused or omitted entirely. These two-digit codes provide additional information about the service performed, helping insurance companies understand the specific circumstances of the procedure.
Common modifier mistakes include using modifier 26 (professional component) when the practice owns the equipment, or failing to use modifier TC (technical component) for equipment-only services. Another frequent error is misapplying bilateral modifiers like 50 or RT/LT for anatomical locations.
The consequences of modifier errors are immediate: claims get denied, payments are delayed, and your staff spends valuable time resubmitting corrected claims. Make sure your billing team understands when and how to apply each modifier code correctly.
Need Help with Radiology Billing Billing?
Book a free consultation to optimize your billing and reduce claim denials.
TALK TO AN EXPERT2. Bundling and Unbundling Errors
The Centers for Medicare & Medicaid Services (CMS) has specific rules about which procedures can be billed together and which cannot. Many radiology practices lose money by either unbundling procedures that should be reported together or bundling services that should be billed separately.
For example, contrast administration is often bundled with certain imaging procedures, but some practices incorrectly bill these components separately. Conversely, some practices fail to bill for separately reportable services like conscious sedation or additional imaging views when appropriate.
Understanding the National Correct Coding Initiative (NCCI) edits and staying current with bundling rules is crucial for proper reimbursement. Regular training and coding updates can help prevent these costly errors.
3. Inadequate Documentation
Documentation is the foundation of successful radiology billing, yet many practices struggle with incomplete or insufficient records. Without proper documentation, even correctly coded procedures can be denied or downcoded during review.
Key documentation requirements include the medical necessity for the procedure, the specific body part examined, any contrast used, and the number of views taken. The radiologist’s interpretation must also be complete and signed within required timeframes.
Poor documentation doesn’t just affect current claims but it can also trigger audits that review historical cases. Implementing documentation improvement programs and regular chart reviews can significantly reduce claim denials and audit risk.
4. Failure to Verify Insurance Coverage
Not verifying patient insurance coverage before procedures is a mistake that can be devastating to collections. Many radiology procedures require prior authorization, and failing to obtain this approval often results in complete claim denials.
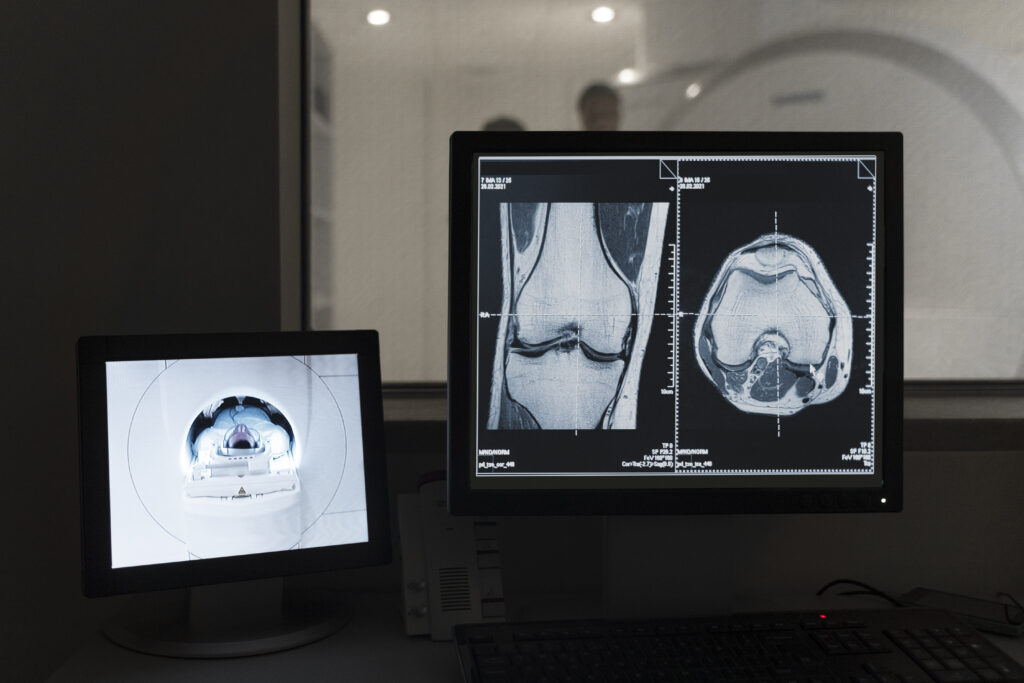
Insurance verification should include checking eligibility, benefits, deductibles, and copayment requirements. For high-cost procedures like MRI or CT scans, understanding the patient’s financial responsibility upfront prevents collection issues later.
Establishing a robust verification process with clear protocols for obtaining authorizations can dramatically improve your first-pass claim acceptance rate and reduce bad debt.
5. Incorrect Anatomical Coding
Radiology procedures are highly specific to anatomical locations, and using incorrect anatomy codes is a common source of claim denials. This includes errors like coding the wrong body part, using non-specific codes when specific ones are available, or failing to specify laterality when required.
For instance, coding a knee MRI as “lower extremity” instead of specifying “knee” can result in denial or reduced payment. Similarly, failing to indicate right or left when examining paired organs often triggers automatic denials.
Investing in anatomy coding training and using coding resources specific to radiology can help reduce these errors. Many practices also benefit from implementing coding checklists for complex procedures.
6. Contrast Media Billing Errors
Contrast administration has specific medical billing rules that are frequently misunderstood. Not all contrast use is separately billable, and the rules vary depending on the procedure and the type of contrast used.
Common errors include billing for contrast when it’s already included in the procedure code, using incorrect contrast codes, or failing to document the medical necessity for contrast enhancement. Some practices also make mistakes with oral versus intravenous contrast billing rules.
Understanding when contrast is separately reportable and ensuring proper documentation of contrast use can recover significant lost revenue for many practices.
7. Ignoring Payer-Specific Requirements
Different insurance companies have varying requirements for radiology billing, and treating all payers the same way leads to unnecessary denials. Medicare, Medicaid, and private insurers each have specific rules about coverage, coding, and documentation.
Some payers require specific modifiers, have different bundling rules, or need additional documentation for certain procedures. Failing to understand these payer-specific requirements results in claim rejections that could have been avoided.
Maintaining payer-specific billing guidelines and training staff on major payer differences can significantly improve clean claim rates and reduce administrative burden.
8. Poor Follow-up on Denied Claims
Perhaps the most costly mistake is failing to properly follow up on denied claims. Many practices write off denials without attempting to correct and resubmit them, leaving significant money on the table.
Effective denial management requires tracking all denials, identifying patterns, and implementing corrective actions. This includes appealing inappropriate denials, correcting and resubmitting claims with minor errors, and addressing systemic issues causing recurring problems.
Practices that implement strong denial management processes often recover 15 to 20 percent more revenue than those that don’t actively pursue denied claims.
Protecting Your Practice’s Revenue
Avoiding these common radiology billing mistakes requires ongoing attention to detail, regular training, and robust quality assurance processes. Consider implementing these strategies:
Regular coding education and updates for your billing team, pre-submission claim review processes, automated insurance verification systems, comprehensive denial management protocols, and regular audits of your billing practices.
Remember that investing in proper billing practices and staff training pays dividends through improved cash flow, reduced denials, and decreased audit risk. The cost of preventing these mistakes is always less than the cost of fixing them after they occur.
By addressing these eight common billing errors, your radiology practice can significantly improve its financial performance while ensuring compliance with ever-changing healthcare regulations. Take the time to evaluate your current processes and implement improvements where needed because your bottom line will thank you.
Need Help With Your Radiology Billing?
Tired of dealing with billing headaches? Medlife makes radiology billing simple and stress-free. Our team handles all the complex coding, documentation, and insurance requirements so you can focus on your patients. Contact us today for a free consultation. Let us show you how easy radiology billing can be.


